PDS has been working with Allerton-Fox and Barr & Barr on the construction of the re-designed Emergency Department for Montefiore Nyack Hospital.
NY Build Conference - March 12th/13th
Our Principal Mike and Senior Project Manager Dan were invited to the NY Build Conference Expo held at the Javits Center in New York City where they spoke to the audience about PDS’s work in Behavioral Health Design. The NY Builds Expo is a two day event that gathers professionals across the design and construction industry. More information on the expo can be found at the website: https://www.newyorkbuildexpo.com
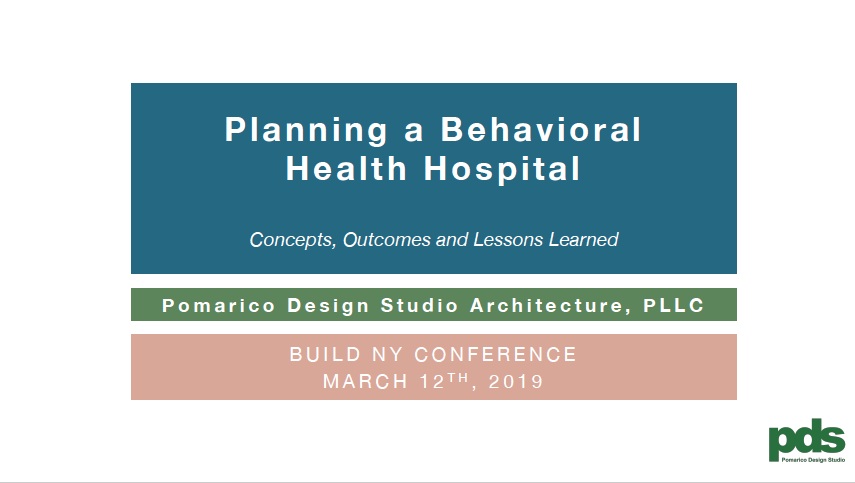
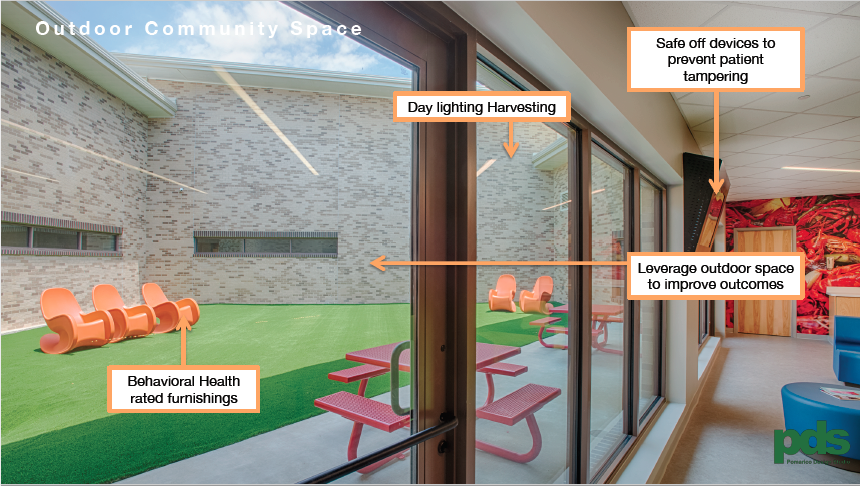
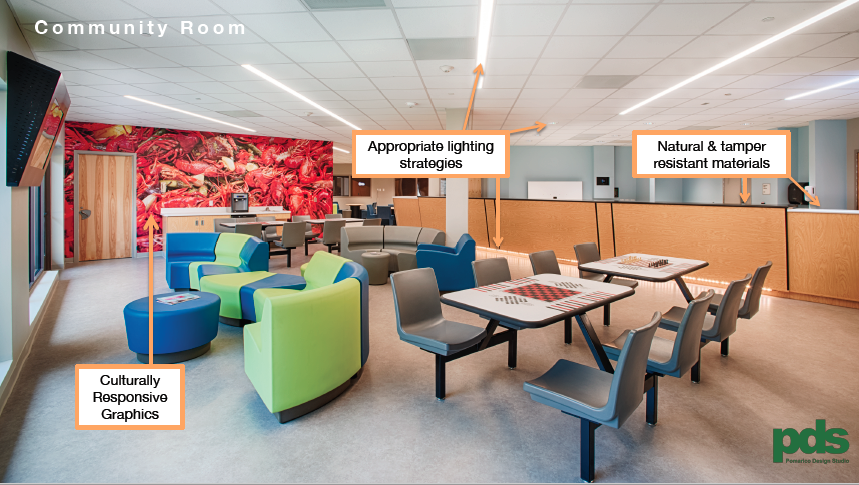
The presentations covered code reviews, concepts, outcomes and lessons learned from several Behavioral Health facilities that PDS has completed in the past few years. Here are a few slides from the presentation.

Lieutenant Governor Kathy Hochul visits Montefiore Nyack DSRIP ED
Bringing in the Community
Mike Pomarico and Stephen Delray presenting at the MMC Weiler ED project to the community.
As Emergency Departments continues to see large volumes of patients, longer wait time, and over crowded spaces, it is necessary to re-think and re-design how a modern emergency department functions.
Last week, our Principal, Mike, and Project Manager, Stephen, engaged the community with the new design and renovation of the Emergency Department at Montefiore Medical Center's Weiler Campus in Manhattan. These community meetings are very important, and as designers we must be very receptive to feedback, concerns, and suggestions amongst the community.
Later on we caught up with Mike and had the opportunity to hear some of his thoughts on the processes of these meetings.
What is the importance of these meetings?
Mike: It is important to the hospital's mission to integrate the community into the delivery of care and to maintain and raise the awareness level to not only improvements that are being made in the continuum of care, but also what choices are available for deliver of care.
What does the client (hospital) get from the meeting?
Mike: The client builds their relationship with the community. They build a sense of trust, the client also convey's their mission to the community and obtains a buy in on their care delivery model. The client also gains valuable information related to patient satisfaction as it pertains to both access and quality of care.
How much pull do they have as stakeholders?
Mike: The community as stake holders are influences whom are able to, through their community board and other social and political associations, broadcast the hospitals mission plans, achievements and care delivery models to a broad base of the community.
How do these meetings effect our design?
Mike: As we present to and participate in the questions and answer portion of the meeting, we have the opportunity to preemptively understand community needs and concerns that may offer potential design adjustments and/or modifications.
ER, Critical Care & Trauma
Pomarico Design Studio has had the pleasure to design and build the Emergency Department and supporting programs at Lake Charles Memorial Hospital. As emergency departments continue to be heavily used, PDS is innovating creative solutions to improve the ED experience. Through strategic planning, collaborating with hospital staff, and innovating the latest health technology, our goal is to create the best environment of care during times of uncertainty.
Take a fly through of the ED + supporting programs at LCMH.
Video Credit: Lake Charles Memorial Health System
“Emergencies don’t stop at the ER door. Memorial is committed to providing everything patients need for critical care and trauma.”